The following text serves as a temporary placeholder, prior to expert moderation
TMS
Moderated by: TBD
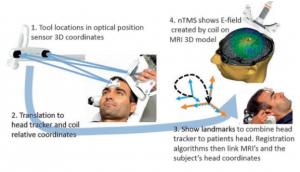
Transcranial magnetic stimulation (TMS) uses a transcranial magnetic field to elicit electro-cortical activation or inhibition. Using this technique, pre-operative functional maps can be created to guide the intra-operative decision-making, also known as navigated TMS (nTMS) (1,2).
Technical Parameters
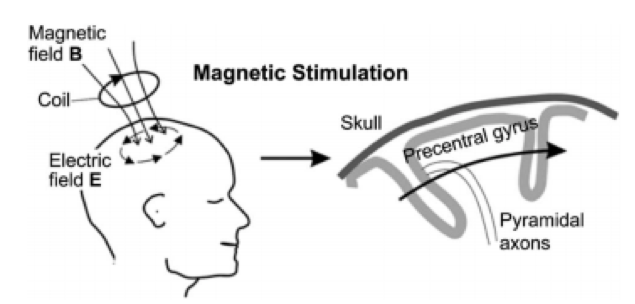
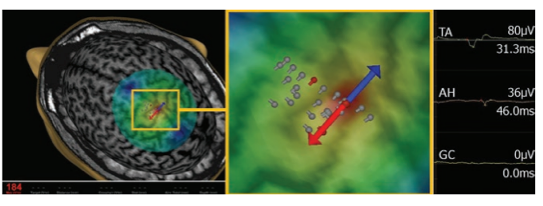
TMS makes use of the principle of electromagnetic induction (1). Using a so-called TMS-coil which has a current running through, a focused magnetic field is created which can penetrate well through the skull to finally induce an electrical field in the brain (Figure 1 and 2) (3,4). Depending on the protocol, activation-based mapping for e.g. motor tasks (single pulse) or inhibition-based mapping for e.g. language tasks (low-frequency repetitive pulse trains) can be facilitated.
TMS is able to reach a spatial resolution of around a centimeter (5). The depth which can be achieved with the electric field is also in the range of centimeters, as the field strength decreases rapidly as a function of tissue depth (6,7). The temporal resolution of TMS is dictated by the duration of the single pulse or stimulus trains, which is often below a single second (5). A full mapping effort can take several minutes, in line with ESM.
Biological Substrate
Similar to ESM which is used in an intra-operative setting, TMS directly stimulates or inhibits cortical areas of interest. Per definition, these areas have to be considered as essential to the observed reaction, and therefore are eloquent areas intra-operatively (8). This in contrast to techniques such as fMRI and MEG, where entire networks underlying a reaction are detected, essential as well as less or non-essential areas.
Intra-operative applicability
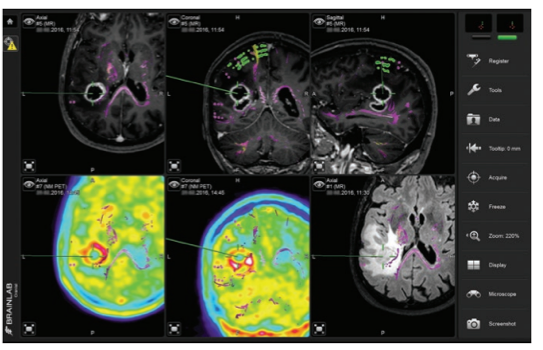
TMS is an inexpensive, non-invasive tool, and portable, which has the ability to identify essential, functional regions prior to awake surgery. Similar to MEG, the pre-operatively acquired TMS-based functional map needs to be registered to and plotted onto the intra-operative MRI, which can be done in the OR-setting prior to surgery (see Figure 3). However, it does not allow for actual intra-operative brain mapping, meaning that intra-operative techniques will remain necessary in concomitance (2). Similar to ESM, TMS carries the risk of pre-operative seizure elicitation (1), in addition to several other minor side-effects such as temporary headache or pain (9).
References
- Tarapore PE, Picht T, Bulubas L, Shin Y, Kulchytska N, Meyer B, et al. Safety and tolerability of navigated TMS for preoperative mapping in neurosurgical patients. Clin Neurophysiol. 2016;
- Ottenhausen M, Krieg SM, Meyer B, Ringel F. Functional preoperative and intraoperative mapping and monitoring: increasing safety and efficacy in glioma surgery. Neurosurg Focus. 2015;38(1):E3.
- Ritaccio AL, Brunner P, Schalk G. Electrical stimulation mapping of the brain: Basic principles and emerging alternatives. Journal of Clinical Neurophysiology. 2018.
- Tarkiainen A, Liljeström M, Seppä M, Salmelin R. The 3D topography of MEG source localization accuracy: Effects of conductor model and noise. Clin Neurophysiol. 2003;
- Sliwinska MW, Vitello S, Devlin JT. Transcranial magnetic stimulation for investigating causal brain-behavioral relationships and their time course. J Vis Exp. 2014;
- Deng Z De, Lisanby SH, Peterchev A V. Coil design considerations for deep transcranial magnetic stimulation. Clin Neurophysiol. 2014;
- Cohen D, Cuffin BN. Developing a more focal magnetic stimulator. part I: some basic principles. J Clin Neurophysiol. 1991;
- Forster MT, Hattingen E, Senft C, Gasser T, Seifert V, Szelényi A. Navigated transcranial magnetic stimulation and functional magnetic resonance imaging: Advanced adjuncts in preoperative planning for central region tumors. Neurosurgery. 2011;68(5):1317–24.
- Machii K, Cohen D, Ramos-Estebanez C, Pascual-Leone A. Safety of rTMS to non-motor cortical areas in healthy participants and patients. Clin Neurophysiol. 2006;
- Krieg SM. Navigated Transcranial Magnetic Stimulation in Neurosurgery. Springer, Cham. 2017