ESM
Moderated by Sadaf Soloukey, PhD-student CUBE, department of Neuroscience and Neurosurgery, Erasmus MC, Rotterdam, the Netherlands.
Electro-cortical Stimulation Mapping (ESM), also known as Direct Electrical Stimulation (DES), is a direct, intra-operative mapping technique which makes use of electrical current to activate or disrupt specific functional areas around the tumor during awake surgery (1,2). For many, ESM is considered the gold standard for intra-operative, functional brain mapping (1,3).
Technical Parameters
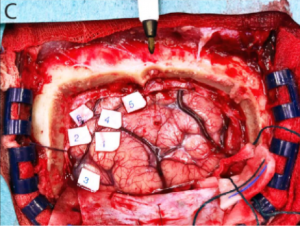
ESM is applied during awake craniotomy surgery, where the patient has the ability to perform simple functional tasks such as finger tapping or word repetition under guidance of a neurolinguistic specialist or neuropsychologist. Using bipolar stimulating forceps, cortical grids or depth electrodes (see also ‘ECoG’ and ‘sEEG’), the surgeon systematically stimulates the exposed cortical surface surrounding the tumor, while the patient is preforming these functional tasks. In case of disruption or change in the patient’s performance during stimulation, that specific area of the cortex is deemed eloquent and is marked, often using physical, numbered cut-outs (see Figure 1). Literature reports great differences in mapping approaches across surgeons and institutions (1). While some use a single stimulation amplitude to cover the full area to avoid electrical after-discharges, others systematically increase the amplitude to maximize amplitude at each cortical site to ensure the absence of eloquent function (1). This has a great influence on the reproducibility of the technique as well as the comparability of the technique’s success across institutions.
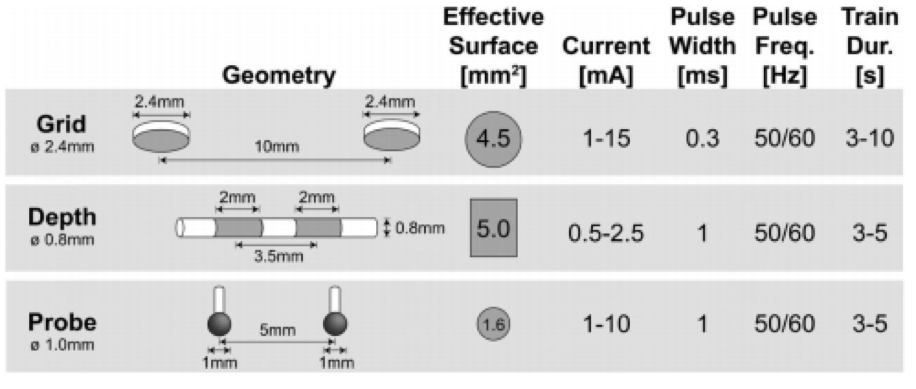
In terms of spatial resolution, ESM is a hard technique to pinpoint, as it is dependent on multiple factors. First, the spatial resolution is dictated by the electrode interface used, including parameters such as electrode diameter, interelectrode distance and stimulation intensities (see Figure 2). What is more, the area of the electrode interfacing with the issue is often not the effective surface which is electrically stimulated. In fact, the combination of relatively unpredictable current spread into the surrounding tissue together with potential electrical after-discharges or even seizure elicitation, make it difficult to determine the area covered by the bipolar stimulation, and increases the risk of false positives. Finally, once stimulated and marked, the spatial resolution is reduced to the surface area of the marker. Therefore, it is fair to estimate spatial resolution of ESM is below a 1 centimeter (1). The duration of the full mapping effort is variable but extensive and depending on the surgeon and the patients, can take multiple minutes (2). In terms of depth penetration, ESM is thought to cover a volume of several millimeters of tissue without actual depth resolution, depending on the parameters such as stimulation amplitude described above (1).
Biological Substrate
ESM makes use of electrical current to evoke both excitation/positive responses (regional movement, dysesthesia, phosphenes) and disruption/negative responses (motor inhibition, speech arrest, anomia). Mapping is biased to spontaneous positive responses, and negative behavioral responses are detected only if the respective function is explicitly tested. This makes ESM a limited technique in terms of functional tasks, similar to fMRI. Only a finite set of functional tasks are suitable to use in combination with ESM and in the surgical setting of an awake craniotomy.
Intra-operative applicability
ESM is an ideal technique for intra-operative application given its inexpensiveness, portability, ease of use and direct feedback, which might explain its wide-spread application as a gold standard during awake surgery. In fact, currently there is no other technique which provides similar direct feedback of cortical functionality in an intra-operative setting. However, it also presents with several considerable limitations. Given its use of electrical current, ESM is prone to false positives or elicitation of seizures, the latter of which can seriously disrupt the surgical workflow (1,2,4). Additionally, ESM is a rather superficial technique, mostly applicable to the surface of the cortex en vue. Intra-operative subcortical stimulation of white matter during tumor resection has been described, although less commonly used and more difficult to interpret (5,6). Finally, the technique has not been standardized, making it difficult to compare ESM-results between surgeons or across institutions (5,6).
References
- Pouratian N, Cannestra AF, Bookheimer SY, Martin NA, Toga AW. Variability of intraoperative electrocortical stimulation mapping parameters across and within individuals. J Neurosurg. 2004;
- Ritaccio AL, Brunner P, Schalk G. Electrical stimulation mapping of the brain: Basic principles and emerging alternatives. Journal of Clinical Neurophysiology. 2018.
- Haglund MM, Berger MS, Shamseldin M, Lettich E, Ojemann GA. Cortical localization of temporal lobe language sites in patients with gliomas. Neurosurgery. 1994;
- Soloukey S, Vincent AJPE, Satoer DD, Mastik F, Smits M, Dirven CMF, et al. Functional Ultrasound (fUS) During Awake Brain Surgery: The Clinical Potential of Intra-Operative Functional and Vascular Brain Mapping. Front Neurosci. 2020;
- Keles GE, Lundin DA, Lamborn KR, Chang EF, Ojemann G, Berger MS. Intraoperative subcortical stimulation mapping for hemispherical perirolandic gliomas located within or adjacent to the descending motor pathways: Evaluation of morbidity and assessment of functional outcome in 294 patients. J Neurosurg. 2004;
- Duffau H. Contribution of cortical and subcortical electrostimulation in brain glioma surgery: Methodological and functional considerations. Neurophysiol Clin 2007;37(6):373–82.